All published articles of this journal are available on ScienceDirect.
Intralipid-Based Phantoms for the Development of New Optical Diagnostic Techniques
Abstract
Intralipid is a material widely employed for the preparation of phantoms for optical imaging and biophotonics applications in medical field. The development of new optical diagnostic equipment in these fields requires the use of well-designed phantoms with optical properties (including scattering and absorption) mimicking those of biological tissues in all the pre-clinical stages of investigations. For this reason, great research effort has been devoted to optically characterize Intralipid and at preparing optimal phantoms. In this short review, we summarize the principal physico-chemical characteristics of Intralipid and the main contributions in the assessment of its scattering and absorption properties. In addition, the most largely used Intralipid-based homogeneous and non-homogeneous phantoms are discussed. Even though other materials are available for the preparation of phantoms, the use of Intralipid still offers an inexpensive and easy-to-use method for preparing phantoms with finely tuned optical properties.
1. INTRODUCTION
In the last years, the popularity of optical techniques as powerful methods for studies in the biomedical field have been continuously increasing [1-9]. Among the other outcomes, biophotonics research has made new approaches available for the development of innovative diagnostic tools [9]. In particular, time-resolved Near-Infrared (NIR) spectroscopy has been demonstrated to be particularly appealing [10-13] for realizing imaging systems aimed at investigating human tissues and bodies, for diagnostic and therapeutic purposes. By using various geometries and experimental set-ups, the propagation of light in opaque media was used to design new approaches and devices enabling to image real opaque systems, such as human tissues and parts of the human body (see Supplementary Materials for a short description of the basic principles of light propagation-related techniques and theoretical descriptions) [14, 15]. The development and assessment of new optical diagnostic equipment require the use of well-designed tissue phantoms in all the pre-clinical stages of investigations [16]. For obtaining phantoms with optical properties mimicking those of biological tissues, Intralipid is largely employed. Intralipid indicates an aqueous suspension of lipid droplets that is sterile and suitable for intravenous feeding of patients and drug delivery [17]. It is also used also as an antidote against anesthetic toxicity and various toxins [18] and as a cardioprotective agent [19].
In the last years, other materials have been adopted for preparing phantoms for reference and calibration tests of optical diagnostic tools and instruments [20, 21], but Intralipid is still an interesting choice because it is easy to handle and has a low price. For these reasons, we believe that it can be interesting to revise the main examples of Intralipid phantoms reported in the literature and the procedures to realize them also with the aim of stimulating new biotechnological research in the field.
In order to give a general but not exhaustive overview of the topic, in this review, we will focus on different phantoms prepared with Intralipid and other additional components usefully employed in preclinical testing of optical diagnostic instrumentation adopting time-resolved techniques developed for breast and brain imaging applications. In particular, we will report on homogeneous and inhomogeneous phantoms in the liquid and solid state. Homogeneous phantoms have been largely used for investigating the performances of the various optical techniques in assessing the optical properties of biological tissues. Inhomogeneous phantoms are strictly required for evaluating optical imaging systems performances. In this framework, there are two main classes of phantoms: phantoms in which small inclusions are present and layered phantoms. The former ones are mainly used for imaging small tumour lesions in different tissues and the latter for brain imaging. We will discuss the general physico-chemical properties of Intralipid, with particular attention to its optical properties, and we will give information about some other additional substances used in the preparation of Intralipid-based phantoms. After this, we will present just some particularly significant Intralipid phantoms which are indicative of the large amount of work available in the literature. Similar consideration has to be done for the cited references, the list is far from being exhaustive, but it is only demonstrative of the large amount of literature available in this field, witnessing the great importance of the topic in the present biomedical research. The results of a survey about recent patents regarding Intralipid phantoms will be also discussed, witnessing, on one hand, the economic importance of these phantoms as testing elements for new medical equipment and, on the other hand, the number of patents devoted at presenting new methods for realizing Intralipid based phantoms.
2. PHYSICO-CHEMICAL PROPERTIES OF INTRALIPID
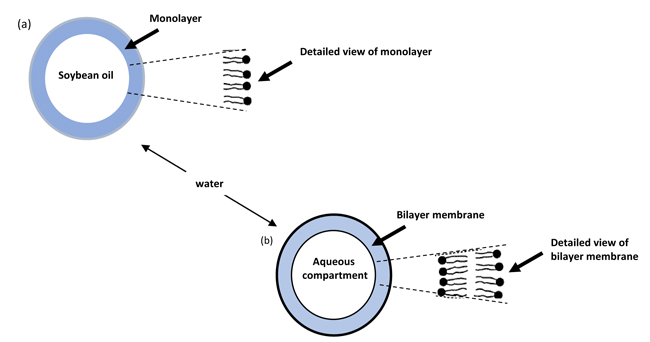
Intralipid (mainly produced by Pharmacia (USA), Fresenius Kabi (Germany), Baxter (USA), Kabivitrum (USA)) is an aqueous suspension of lipid droplets that is sterile and suitable for intravenous feeding of patients. It is available as Intralipid-10%, Intralipid-20% and Intralipid-30% (the percentage indicating the relative amount of lipids; for instance, 10% indicates 10 g of lipid per 100 ml of suspension). The constituents of Intralipid-10% in a 500 mL (497.75 g) bottle according to the manufacturers are soybean oil (50 g), lecithin (6 g), glycerin (11.25 g), water (430.5 g). Intralipid suspension is composed mainly by quasi-spherical colloidal particles with size falling in the range 25-625 nm, consisting of soybean oil encapsulated within a monolayer membrane of lecithin with a thickness of approximately 2.5-5 nm [22]. The glycerin is dissolved into individual molecules in the water. A description of the colloidal particles as concentric spheres can be reasonably adopted. In Intralipid-10%, approximately half of the amount of lecithin is used for encapsulating the soybean oil, and the excess of lecithin forms small bilayer vesicles Fig. (1).
Some parameters largely investigated in Intralipid solutions are the particle average diameter, size distribution and polydispersity because they influenced the delivering speed of the emulsion and also its efficiency in drug release. Electron microscopy permits determination of both the size and the shape of the scattering particles in Intralipid-10%. Van Staveren et al. [22] reported the results obtained by using a magnification of 18000x at 100 kV in a Philips EM 420 electron-microscopy. They showed the size differences in Intralipid-10% particles and their generally spherical shape. A shell structure was not apparent, thus proving that a sharp boundary (in the case of a bilayer membrane) between lecithin and soybean oil was absent. Hence, they concluded that the layer of lecithin was a monolayer. The measured particle sections were classified into 14 particle diameter classes (see Fig. (7) of Ref. [22]) in Intralipid-10%. The mean particle diameter of this distribution was 97 + 3 nm. A form factor (Perimeter Eccentricity (PE)) was computed for the particle sections. This form factor for an area A with perimeter s was defined according to the following Eq. (1).
 |
(1) |
The closer the form factor is to 1 (for any non-spherical shape PE < 1), the closer the particles are to a spherical shape. A plot of the form factor versus the particle diameter [22], allowed the authors to affirm that a spherical shape can be reasonably assumed.
As reported by Rotenberg et al. [23] Quasi-elastic Light Scattering (QLS) measurements can also be used for the evaluation of the particle sizes in various Intralipid samples. Measurements were carried out on a Malvern photon correlation spectrometer (Model 4700), equipped with an Argon laser operating at λ = 488 nm. All the samples were diluted 100-2000-fold in 2.5% glycerol prior to being measured. Dilution of the samples in either 2.5% glycerol, in 0.15 M NaCl or water did not affect the size of the particles in the suspension. Measurements were carried out at 25°C, both at a fixed angle of 90 degrees, or multiple angles (45-105 degrees). The results indicated that large emulsion particles with mean diameters ranging from 265 nm in 10% Intralipid to 400 nm in Intralipid-30% were present. These data are consistent with the previous reports on QLS size measurements of particles from 10% and 20% emulsions of various commercial sources [24, 25]. Electron microscopy viewing supported the QLS measurements and ruled out the presence of even smaller aggregates (dimension << 50 nm) which would not have been detected by light scattering analysis.
Intralipid particle size was also measured by using Photon Correlation Spectroscopy (PCS) [26]. This is a laser-light scattering technique that uses fluctuations in scattered light intensity to measure the velocity of Brownian diffusion of small particles that is influenced by the particle diameter. Using PCS, it is possible to determine particle average diameter, size distribution and polydispersity. This technique is also able to measure zeta-potential when combined with electrophoresis. For Intralipid -20% an average diameter ranging between 309.5 + 5.3 and 344.0 + 12.9 nm was measured in dependence of the batch. In the paper of Komatsu et al. [26] also data for zeta-potential are discussed. PCS technique was also employed by Li and Caldwell [27] for determining differences in particle size between Intralipid-10% and -20%. They found that the Intralipid-10% emulsion has an average particle size (average diameter: 265 nm) smaller than its 20% analogous (average diameter: 367 nm) although the manufacturer gives the same value for both of them (average diameter: 500 nm).
Ferezou et al. [28] investigated Intralipid-10% by using electron microscopy. They evidenced the coexistence of artificial chylomicrons (mean diameter: 260 nm) and liposomes (average diameter: 43 nm). The size (mean diameter: 43 nm) of the liposomes present in Intralipid-10% is smaller than that usually assumed.
3. OPTICAL PROPERTIES OF INTRALIPID
As said before, Intralipid is one of the most extensively studied reference materials in the biomedical optics community and for this reason, its optical properties have been investigated in a number of papers. Here, we will report the results discussed in some of the most cited ones [22, 29-31].
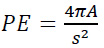
As well-known biological tissues can be considered as turbid media when light propagates inside them. The light propagation can be essentially described taking into account four optical parameters: the absorption coefficient, μa (the inverse of the mean free path before absorption event), the scattering coefficient, μs (the mean number of photon scatters per unit length), the anisotropy g-factor (the mean cosine of the scattering angle) and the refractive index n (the ratio between the speed of light in the vacuum and in the medium). Usually, μs and g are combined in the reduced scattering coefficient μs’ which is defined as μs’= (1-g) μs. Another parameter that can be used for taking into account all these quantities is the diffusion coefficient, D, that can be expressed Eq. (2) as:
 |
(2) |
The numerical values of the above-introduced optical parameters for soft human tissue are reported in Table 1.
Table 1.
|
Optical Parameter |
Value for Soft Human Tissue |
|---|---|
| Absorption Coefficient |
~ 0.05 cm-1 in the near infrared wavelength region |
| Scattering Coefficient |
1-5 cm-1 for 600-1300 nm wavelength |
| Anisotropic g-Factor |
0.95-0.98 |
| Refractive Index | ~ 1.4 |
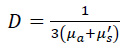
For describing optical properties of Intralipid, Driver et al. [29] introduced an effective attenuation coefficient given by the following expression in Eq.(3):
 |
(3) |
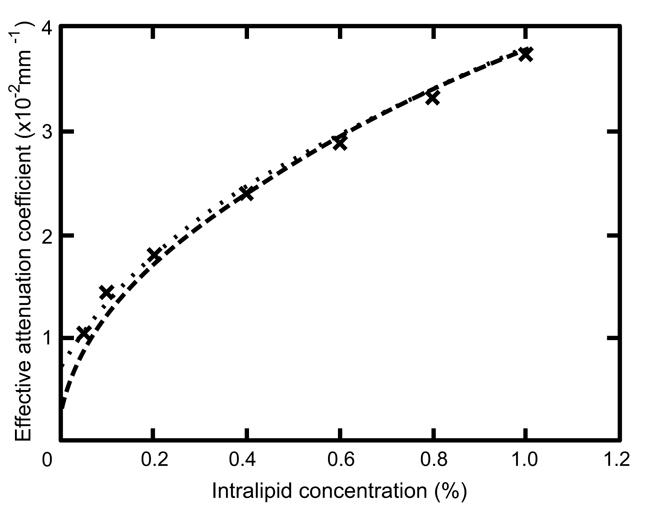
In the paper by Driver et al. [29], aqueous suspensions of Intralipid-20% were examined. The mean particle size was measured and found to be 444 + 84 nm. The effective attenuation coefficient of Intralipid solutions at concentrations ranging from 0.05 to 1.0% in volume was determined at a wavelength of 630 nm by measuring the space irradiance at different source-detector distances using an isotropic source and detector submerged in the solution. In Fig. (2), the main results are reported.
Van Staveren et al. [22] measured the absorption, scattering, and anisotropy coefficients of the fat emulsion Intralipid-10% at 457.9, 514.5, 632.8, and 1064 nm. The main results are reported in Table 2 along with results from other studies.
Flock et al. [30] extended the measurements of the absorption and reduced scattering coefficients from 460 to 690 nm and the total attenuation coefficient from 500 to 890 nm. These measurements showed that, for stock Intralipid- 10%, the absorption coefficient varied from 0.015 to 0.001 cm-1 between 460 and 690 nm, the reduced scattering coefficient was in the 92 to 50 cm-1 range between 460 and 690 nm, the total attenuation coefficient changed from 575 to 150 cm-l between 500 and 890 nm, and the average cosine of the scattering angle was in the 0.87 to 0.82 range between 460 and 690 nm.
In 2014, Spinelli et al. [31] reported a multi-center study aimed at accurately characterizing the optical properties of Intralipid at NIR wavelengths. Nine research laboratories adopting different measurement techniques, instrumental set-ups, and data analysis methods determined the optical properties and relative uncertainties of Intralipid suspensions. The authors reported intrinsic reduced scattering coefficient of Intralipid-20% with an uncertainty of about 1%.
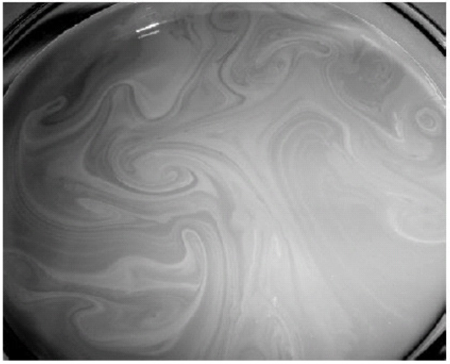
An interesting feature of Intralipid was evidenced by Bodenschatz et al. [32] that considered the layering properties of this substance that is generally assumed to have homogeneous optical properties. The image of a sample obtained by using Intralipid and ink is shown in Fig. (3): the formation of a surface layer is evident. The surface layer is present also when no absorber is used, but in this case, is less evident to the eye. Using frequency domain reflectance and an analytical solution for a two-layer media, Bodenschatz et al. investigated the characteristics of this surface layer when suspensions with different Intralipid concentrations are used [32]. The obtained results indicated that a highly scattering layer is formed and, thus, has to be taken into account when using Intralipid phantoms. In order to minimize the surface layer effects, the authors also suggested to avoid long-standing times for Intralipid before measurements.
The results so far discussed are representative of a very large number of studies aimed at best characterizing the optical properties of Intralipid [33-41]. Due to the ready availability, low cost, long-term stability and batch-to-batch reproducibility of Intralipid, it can be considered a fundamental compound for preparing phantoms for the calibration and performance assessment of optical spectroscopy instrumentation for optical imaging, even if some attention has to be paid to the fact that Intralipid cannot be rigorously considered an optical standard [31, 38].
4. INTRALIPID-BASED PHANTOMS
In this section, the characteristics of the more largely used homogeneous and non – homogeneous Intralipid based phantoms are reported. For the fabrication of these phantoms, Intralipid is generally used as scattering agents, some other materials are used as absorbing agents and some substances are sometimes employed as a hardener. In the Supplementary Materials, a short note about the principal properties of inks and hardeners is reported. It has to be underlined that Intralipid phantoms have high stability, resulting to be of some months for liquid phantom and up to one year for solid ones, when some simple precautions are taken in their storage [42-45].
4.1. Liquid Homogeneous Phantoms
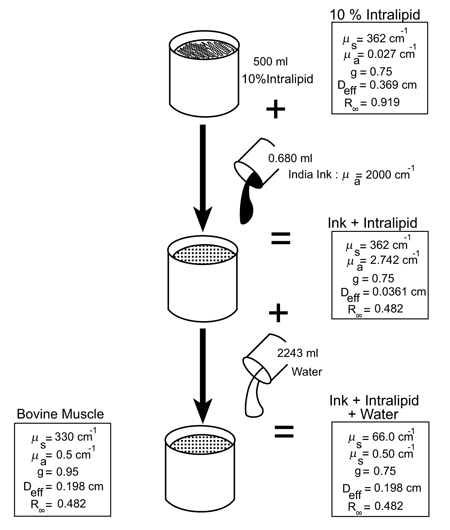
Given the above mentioned characteristics of Intralipid suspensions, many different researchers adopt it for preparing liquid homogeneous tissue phantoms useful for the development of time-resolved imaging systems [20, 31, 46-50]. A description quite accurate about the preparation of this kind of phantoms is reported in Ref. 30. As said before, in that paper, Flock et al. preliminarily collected data on optical coefficients of Intralipid measured at 633 nm (Table 1 of [30] and after extended the measurements of the absorption and reduced scattering coefficients from 460 to 690 nm and the total attenuation coefficient from 500 to 890 nm. Using these measured data, they described the different steps of preparation of an optically tissue-equivalent phantom consisting of Intralipid and black India ink.
They used the similarity relations [51, 52], which can be formulated to show that two media (labelled with subscripts 1 and 2) will exhibit “similar” diffuse reflectance when:
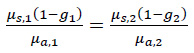 |
(4) |
According to Flock et al., this relation predicts that a medium with g = 0, μa = 1 mm-1 and μs = 9.5 mm-1 will show a reflectance similar to that of a medium with g = 0.5, μa = 0.5 mm-1 and μs = 9.5 mm-1. Eq. (4) is valid if μs(1-g) » μa, for both the media. This condition is necessary because, in the derivation of Eq. (4), it is assumed that the radiance within the medium is linearly anisotropic. Flock et al. [30] used Eq. (4) to design a tissue-like optical phantom consisting of Intralipid and a purely absorbing medium whose characteristics are reported in Fig. (4). The authors assumed that the black India ink acts as a pure absorber even though a molecular dye would be a better choice.
4.2. Solid Homogeneous Phantoms
A recipe largely used for easily preparing solid homogeneous phantoms was proposed by Cubeddu et al. [53]. They suggested that it is possible to prepare this kind of solid phantom by using agar, Intralipid and black ink. The preparation procedure is fast and easily implemented with standard laboratory equipment. A highly purified agar powder is dissolved in distilled water at 1% concentration and heated up to the melting temperature (95 °C) using a microwave oven. The agar solution alone has negligible absorption and very low turbidity. Thus, the desired optical properties of the phantom are obtained by adding appropriate amounts of Intralipid as scattering medium, and India ink as absorbing medium, taking into account that agar induced a systematic decrease in the μs’ value. In [49], all the useful indications about the further steps for obtaining solid phantoms are given. The samples were placed in small transparent plastic boxes (height = 5 cm, width = 5 cm, depth = 2 cm) for the initial optical characterization of the phantom medium that was performed by using time-resolved transmittance experimental set-up. The proposed phantom was characterized by good overall repeatability with a maximum variation of the optical properties < 3% and a standard deviation < 1% of the mean value. All the phantoms were prepared from the same bottles of Intralipid and ink. The authors showed also that it was possible to accurately tune the optical properties in a well-controlled way [53]. These phantoms were also stable for a two months period if stored at room temperature in closed containers.
Many other authors [54-57] used similar phantoms, instead of agar, acrylamide was employed as a hardener by some researchers [58].
4.3. Inhomogeneous Phantoms
When inhomogeneous phantoms have to be prepared three different approaches are usually adopted: liquid-liquid, liquid-solid, and solid-solid configurations, each of them presenting peculiar advantages and disadvantages [59]. Liquid-liquid phantoms are usually constituted by placing a liquid sample (generally prepared with Intralipid and ink) in a small glass or plastic container suspended within another homogeneous medium. Using the liquid-liquid approach, it is possible to change the optical properties of the inclusion and hosting medium in a very easy way. Moving the inclusion inside the hosting medium and preparing a homogeneous reference sample is also easily done in these phantoms. The main problem regards the presence of light guiding effects in the walls of the small container.
For the liquid-solid phantoms agar or polyacrylamide are used for preparing a solid inclusion. This kind of samples can be handled more easily and the change of the inclusion characteristics is simple and light-guiding effects are not present. However, the tuning of optical properties is more difficult because different preparations are necessary for the liquid and solid phases and the refractive index mismatch between the solid inclusion and the liquid medium has to be taken into account.
Solid–solid phantoms can be an optimal choice, but they have fixed characteristics that cannot be changed. For this reason, they are useful only in well-defined situations.
The above described procedures for solid homogeneous phantoms can be adopted for preparing inhomogeneous ones in different ways [53]. For example, holes can be fabricated in a homogeneous agar matrix and it is possible to fill them with solutions having different optical properties in order to mimic a mass embedded in a healthy tissue for controlling imaging optical technique performances. Solid inclusion can be inserted in a liquid medium [60]. In this case, no artifacts due to the solid-liquid interface are present, since the agar matrix is mainly made of water and there is no refraction index mismatch at the solid-liquid interface.
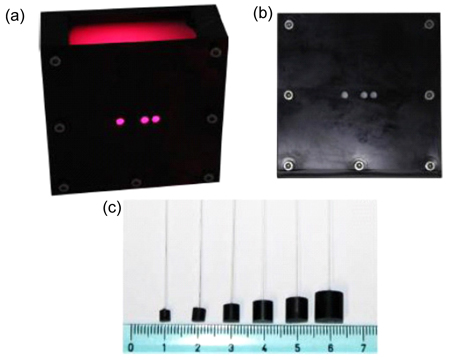
Within the framework of the European nEUROPt Project, an inhomogeneous phantom based on the suspension of black Polyvinyl Chloride (PVC) cylinders within a water suspension of Intralipid and ink was proposed [59]. In Fig. (5), a photograph of this phantom is reported. A scattering cell made of black PVC is a suitable container to prepare liquid phantoms. Photons hitting the black walls are reflected or absorbed and guiding effects are not present. Boundary conditions can be precisely considered both in the Monte Carlo (MC) simulations and with analytical models. The container has small transparent windows that allow the light to enter into the diffusive medium and the diffused light to be collected. Different distances for collecting light are available by considering the different transparent windows. Small black PVC cylinders with different sizes (Fig. 5) immersed in the liquid phantom were used for simulating absorbing objects. The PVC cylinders were held by a rigid metallic wire (0.5-mm music wire) painted white in order to reduce the perturbation. The characteristics of this phantom were carefully investigated by using MC simulations and analytical solutions of the diffusion equation and it was experimentally validated by comparing time-resolved measurements with the results of MC simulations.
4.4. Bilayer Phantoms
Among the inhomogeneous Intralipid-based phantoms, the preparation of multilayer structures useful for developing optical applications for the brain-skull-skin of the human head for the measurement of blood oxygenation in the brain deserves special attention.
A first approach exploits solid phantoms made of agar or other hardener substances like gelatin, Intralipid, and ink for reproducing multilayer structures, by means of different subsequent depositions [60]. In this case, two-layered gelatin phantoms (230x230x55 to 70 mm) were fabricated with thicknesses of the upper layers equal to 10 or 15 mm. The employed base material was a gelatin solution, that can be considered as a transparent material. By adding Intralipid as the scattering agent and greenish-brown ink as absorber, optical coefficients of human layered tissue were simulated. Further details about the preparation protocol are available in [60].
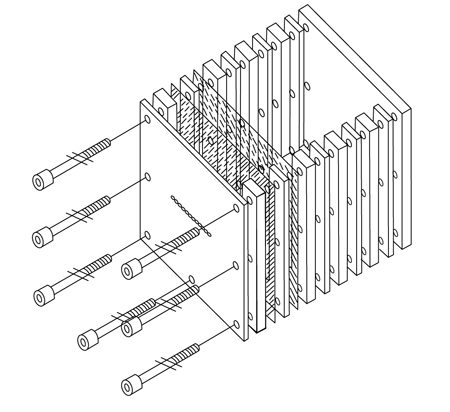
An alternative approach was proposed in 2004 by Del Bianco et al. [61]. It consists in preparing a phantom using Intralipid aqueous suspensions with known absorption and reduced scattering coefficients and thin membranes for separating layers with different optical properties. In Fig. (6), a schematic view of the proposed phantom is reported [61, 62]. The cell was fabricated by using black polyvinyl chloride (refractive index 1.54). A thin layer was placed between the spacers to separate aqueous suspensions (refractive index 1.33) with different optical properties. The spacers were sealed with a thin film of silicone and kept together by screws. Small transparent windows (the small circles in the front wall in Fig. (6) were used to send light to the diffusive medium and to collect the diffuse reflectance at different distances from the light source. The windows were made of polished Plexiglas layers. In addition to Intralipid used as scattering medium, India ink or Cresyl blue were employed as absorbers. The cell was 115 mm high, 100 mm wide, and 60 mm thick. The thickness and the material for the membrane were carefully chosen. In fact, the membrane should separate volumes with different optical properties without introducing appreciable perturbations on light propagation. In particular, a 23-μm thick film of Mylar was chosen. In [61, 62] all the details of a complete characterization are also reported.
5. SURVEY ON PATENTS
Given the importance of Intralipid in the preparation of phantoms for designing and testing the applications of optical methods in medical fields, we examined also the deposited patents concerning Intralipid phantom preparation using Google Patents and Scopus Patents. Using as descriptors the words “Intralipid phantoms” some thousands of papers were found (1994-2018). The largest part of them regards the development of new optical methods and systems, involving the bare use of Intralipid phantoms in the testing step before the use in clinics, thus confirming very large use of this compound in biophotonics research and the economic relevance of the use of Intralipid-based phantoms in this crucial preliminary step. By refining the survey adding the word “preparation” to the descriptors, one hundred patents are still present. After reading the title, summary or report, as inclusion criteria, and avoiding duplicate a small number of patents remains to be considered [63-66]. This confirms that there is still room for realizing new methods aimed at preparing Intralipid-based phantoms with optical and physical properties properly suited for testing equipment with increasing performances. The most representative and well-characterized patent product is the one due to Frangioni and De Grand [63] that mimics any desired tissue and can be imaged using one, two, or more (e.g., four) different imaging modalities (e.g., X-ray Computed Tomography (CT), Positron Emission Tomography (PET), Single Photon Emission Computed Tomography (SPECT), and Near-Infrared (NIR) fluorescence) simultaneously.
CONCLUSION
In this short review, the main properties of Intralipid together with the characteristics of the more generally used Intralipid- based homogeneous and non-homogeneous phantoms have been reported. From this rapid and not exhaustive survey, it is clearly evident that Intralipid phantoms can still play a relevant role in the development, validation and translation of biophotonics technology in the medical field. In fact, other approaches [67-70] result to be more expensive and difficult to handle notwithstanding new methods recently developed to facilitate the fabrication of tissue phantoms for diagnostic and therapeutic purposes.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
Supplementary material is available on the publishers Website along with the published article.


